Menstrual Period Disorders: Causes, Symptoms, and Effective Treatment Options
Learn about the causes, symptoms, and treatment options for menstrual period disorders. Understand how hormonal imbalance, lifestyle, and medical conditions affect menstrual health.
Causes, Symptoms, and Treatment of Menstrual Period Disorders
What Are Menstrual Period Disorders?
Menstrual period disorders are common conditions that affect the regularity, flow, and overall pattern of a woman’s menstrual cycle. These disorders can result from hormonal imbalances, lifestyle habits, or underlying medical conditions. Understanding the causes and symptoms of menstrual irregularities is essential for proper diagnosis and effective treatment.
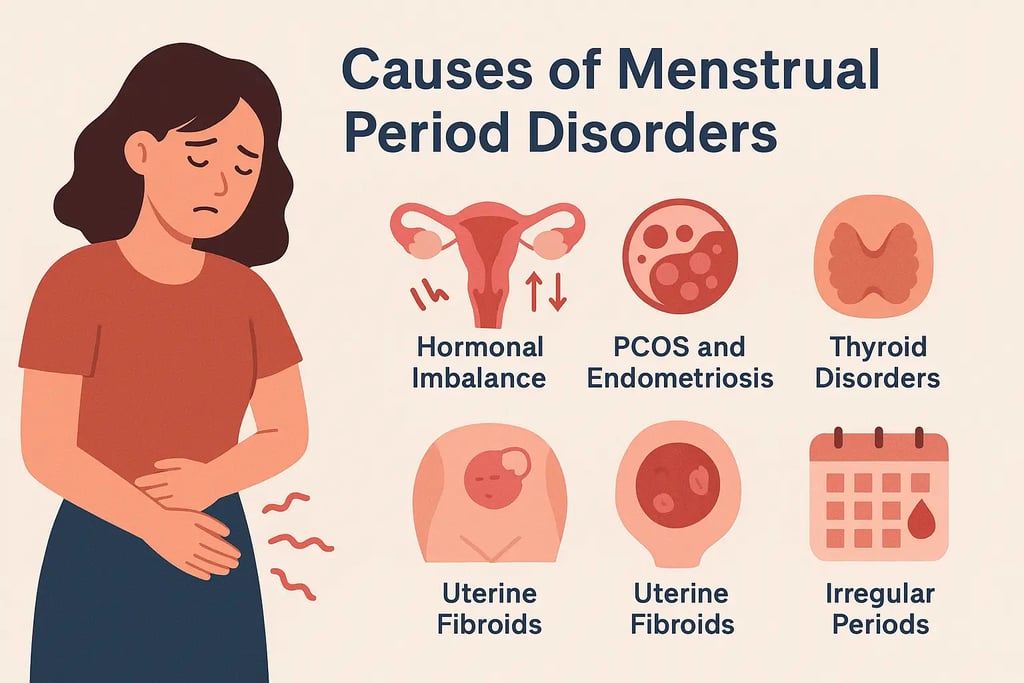
Causes of Menstrual Period Disorders
Several factors contribute to menstrual period disorders, ranging from hormonal changes to chronic health issues. Here are the most common causes:
1. Hormonal Imbalance
Fluctuations in key reproductive hormones such as estrogen and progesterone are among the leading causes of irregular menstrual cycles. When these hormones are disrupted, women may experience conditions such as:
Amenorrhea: Complete absence of menstruation.
Menorrhagia: Heavy or prolonged menstrual bleeding.
Oligomenorrhea: Infrequent or light periods.
2. Polycystic Ovary Syndrome (PCOS) and Endometriosis
Two major reproductive disorders—PCOS and endometriosis—significantly impact menstrual health:
PCOS causes multiple ovarian cysts due to hormonal imbalance, leading to irregular or missed periods.
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, causing severe cramps, heavy bleeding, and pelvic pain.
Both conditions require timely medical evaluation and ongoing management.
3. Thyroid Disorders
The thyroid gland regulates many bodily functions, including menstrual cycles.
Hypothyroidism (underactive thyroid) can cause delayed or absent periods.
Hyperthyroidism (overactive thyroid) may lead to lighter or more frequent cycles.
Proper thyroid management is crucial for restoring menstrual balance.
4. Uterine Fibroids
Uterine fibroids are non-cancerous growths in the uterus that can cause heavy bleeding, pelvic discomfort, and prolonged menstrual cycles. Depending on their size and location, fibroids may require medication or surgical removal.
5. Lifestyle Factors
Everyday habits can strongly influence menstrual regularity.
High stress levels disrupt hormonal balance.
Sudden weight changes (gain or loss) affect estrogen production.
Excessive physical activity, particularly among athletes, can suppress ovulation and cause missed periods.
6. Medications and Birth Control
Certain birth control pills and medications such as anticoagulants or antidepressants can alter menstrual cycles. While hormonal contraceptives are often used to regulate periods, they may initially cause temporary irregularities.
Understanding these diverse causes helps in identifying the root of menstrual disorders and seeking appropriate treatment early.
Symptoms of Menstrual Period Disorders
Menstrual disorders manifest through a range of physical and emotional symptoms that can interfere with daily life.
1. Irregular Menstrual Cycles
Cycles shorter than 21 days or longer than 35 days.
Missed, delayed, or unpredictable periods.
Light or excessively heavy menstrual flow.
2. Heavy or Prolonged Bleeding (Menorrhagia)
Unusually heavy bleeding lasting more than seven days can lead to fatigue, anemia, and other health issues.
3. Painful Periods (Dysmenorrhea)
Intense abdominal or back pain during menstruation can significantly reduce productivity and quality of life.
4. Physical Symptoms
Bloating and abdominal discomfort
Fatigue and general weakness
Breast tenderness and nausea
5. Emotional Symptoms
Hormonal changes during the menstrual cycle can cause:
Mood swings
Irritability
Anxiety or depression
Persistent or severe symptoms should not be ignored. Consulting a gynecologist can help identify the underlying cause and ensure timely treatment.
Treatment Options for Menstrual Period Disorders
Treatment for menstrual period disorders depends on the specific cause, severity, and overall health of the individual. Common approaches include:
1. Medical Treatments
Hormonal therapy: Birth control pills, hormone-releasing IUDs, or progesterone therapy help regulate cycles and control heavy bleeding.
PCOS and thyroid medications: Specific drugs target hormonal imbalances to restore normal menstrual function.
Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce menstrual cramps and discomfort.
2. Surgical Treatments
When medical therapies are ineffective, surgical options may be necessary:
Laparoscopy: Minimally invasive procedure for endometriosis or cyst removal.
Myomectomy or hysterectomy: For severe fibroids or uterine abnormalities causing heavy bleeding.
3. Lifestyle Modifications
Stress management: Practices like yoga, meditation, and deep breathing reduce stress-induced irregularities.
Balanced diet: Consuming iron-rich foods, healthy fats, and vitamins supports hormonal balance.
Regular exercise: Helps maintain a healthy weight and improves overall reproductive health.
A holistic approach combining medical care with healthy lifestyle changes is most effective for managing menstrual period disorders.
When to Seek Medical Help
If you experience persistent irregularities, excessive bleeding, or severe menstrual pain, it’s important to consult a healthcare professional. Early diagnosis ensures timely intervention and helps prevent complications such as infertility or chronic anemia.
Conclusion
Menstrual period disorders are common but manageable with proper care. By understanding their causes, recognizing symptoms early, and adopting suitable treatments, women can maintain optimal menstrual health and overall well-being. Regular checkups, a balanced lifestyle, and open communication with healthcare providers are key to achieving a healthy and predictable menstrual cycle.
